Dr. Henry CY Cheung, Dr Lo Ho Yin and Dr Loletta So
Department of Medicine
Pamela Youde Nethersole Eastern Hospital
Mr Wong was admitted for his fourth episode of blood stained sputum in November 2006.
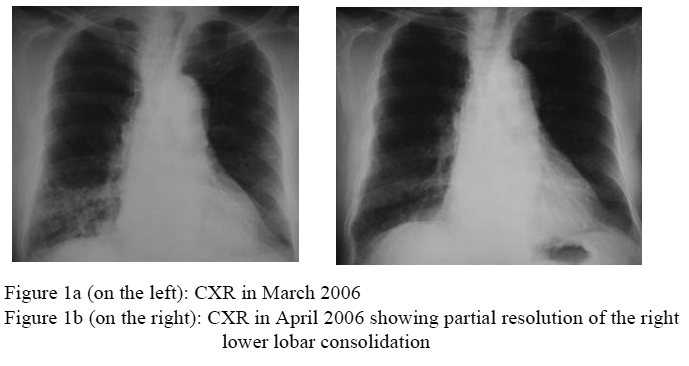
He was an 84-year-old ex-smoker and ex-drinker. He enjoyed good functional status. He had known history of chronic obstructive pulmonary disease, hypertension with mild renal impairment, ischaemic heart disease with heart failure and Parkinson’s disease. His previous three episodes of haemoptysis were in March, June and August of 2006. They were associated with worsening of cough, increase sputum production, mild shortness of breathe. He did not have fever, chest pain or constitutional symptom. There was also no relevant travel, contact or clustering history. Physical examination revealed inspiratory crepitation over his right lower chest. Right lower lobe consolidation was present in CXRs in all the four episodes. A course of Amoxicillin + Clavulanic acid (Augmentin) and Transaminic acid were commended in all the episodes and his symptoms did subside for several weeks or even months. An interval CXR in April also showed the right lower lobe consolidation was resolved partially (Figure 1a & b). However, the subsequent CXRs revealed persistent consolidation over the right lower lobe (Figure 1c, d & e). His baseline blood tests including complete blood picture, liver and renal function test were all unremarkable. His sputum was negative for bacterial culture, acid fast bacillus and cytology all along.
Further enquiry revealed he had choking occasionally. Oral examination also revealed poor oral hygiene with the presence of multiple dental caries.
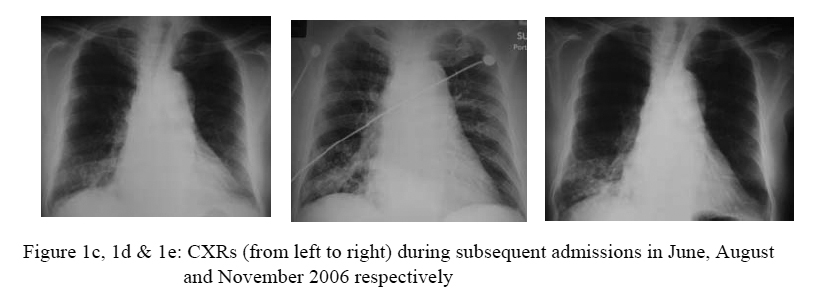
Further work-up included a contrast CT thorax, which showed right lower lobe consolidation and a calcified lesion in his right lower bronchus (Figure 2).
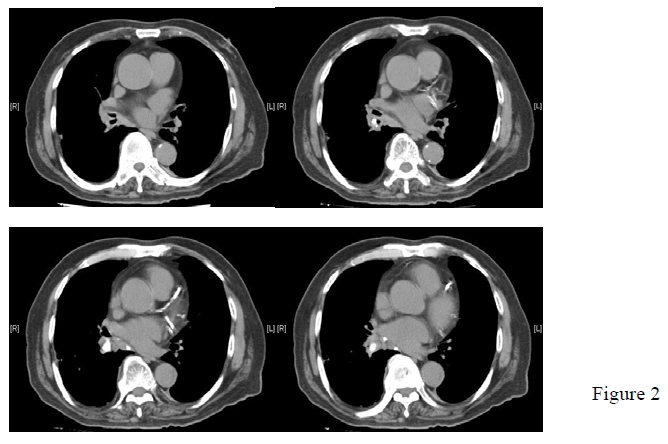
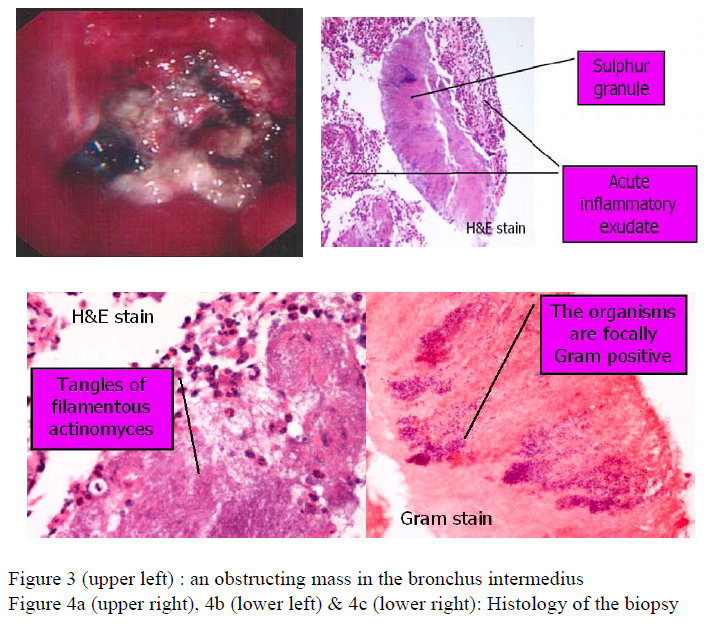
We proceeded to fibreoptic bronchoscopy. It showed an obstructing mass in the bronchus intermedius, with a necrotic-like surface and surrounding inflammed mucosa (Figure 3). Culture of bronchial aspirate yielded several bacteria, including Enterbacter/Serratia species, Coagulase negative Staphylococcus, Alpha-haemolytic Streptococci, Neisseria species and Prevotella species. Cytology, acid fast bacillus and fungal culture were negative. Histology of the biopsy from the mass in bronchus intermedius found acute inflammatory changes and several sulphur granules (figure 4a, b & c). Overall, the clinical picture and histological finding were compatible with endobronchial actinomycosis. The calcified lesion in bronchus intermedias may be a foreign body or a broncholith. Both are known to be associated with endobronchial actinomycosis.
He was treated with 4 weeks of IV Penicillin G, followed by oral Amoxicillin. Some advice was given by the speech therapist to decrease the risk of aspiration. Besides that, root extraction was arranged by the dental surgeon. The mass in bronchus intermedias was found much reduced in size during a reassessment FOB 3 months later.
Actinomycosis is a chronic infection caused by Actinomyces spp. (not fungus), which is an anaerobic-to-microaerophilic, gram positive filamentous rod. Associated or risk factors of endobronchial actinomycosis includes age of 30-50 year old, male (M:F = 2-4:1), underlying respiratory disorders (such as COPD and bronchiectasis), alcoholics, poor oral hygiene, dental & facial disease and aspiration. Actually most of these were present in Mr Wong.
Diagnosis can be confirmed by Gram stain of pus, culture of pus or biopsy specimens or demonstrating sulphur granules in pus or biopsy specimens. Sulphur granule is the pathological hallmark of actinomycosis. Macroscopically, they are ~0.1-1 mm yellowish particles. Microscopically, they are actually conglomerates of filamentous actinomycete microcolonies surrounded by tissue reaction material.
Treatment usually consists of prolonged course of Penicillin for 6-12 months.
***********************************************************************
The second case presented by Dr Grace Law of Kwong Wah Hospital is one of the previously presented cases in the Clinical Meeting of Hong Kong Thoracic Society. For details, please refer to HKTS Newsletter: Sep/Oct 07, Volume 17, Number 3, Page 4 -10.

